“深部脑刺激”的版本间的差异
| 第177行: | 第177行: | ||
== Research == | == Research == | ||
=== Chronic pain === | === Chronic pain === | ||
| − | Stimulation of the [[periaqueductal gray]] and [[Periventricular nucleus|periventricular gray]] for [[Pain#Nociceptive|nociceptive pain]], and the [[internal capsule]], [[ventral posterolateral nucleus]], and [[ventral posteromedial nucleus]] for [[Pain#Nociceptive|neuropathic pain]] has produced impressive results with some people, but results vary. One study<ref name = Young>{{cite journal|authors = Young RF & Brechner T|title = Electrical stimulation of the brain for relief of intractable pain due to cancer|journal = Cancer|volume = 57|year = 1986|issue = 6|pages = 1266–72|pmid = 3484665|doi=10.1002/1097-0142(19860315)57:6<1266::aid-cncr2820570634>3.0.co;2-q| doi-access = free}}</ref> of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.<ref name="Johnson">{{cite book|authors = Johnson MI, Oxberry SG & Robb K|chapter = Stimulation-induced analgesia|pages = 235–50|editor = Sykes N, Bennett MI & Yuan C-S|title = Clinical pain management: Cancer pain|edition = 2nd|isbn = 978-0-340-94007-5|publisher = Hodder Arnold|location = London|year = 2008}}</ref> DBS has also been applied for [[phantom limb pain]].<ref>{{cite journal|vauthors = Kringelbach ML, Jenkinson N, Green AL, Owen SL, Hansen PC, Cornelissen PL, Holliday IE, Stein J, Aziz TZ|title = Deep brain stimulation for chronic pain investigated with magnetoencephalography|journal = NeuroReport|volume = 18|issue = 3|pages = 223–28|date = February 2007|pmid = 17314661|doi = 10.1097/wnr.0b013e328010dc3d|citeseerx = 10.1.1.511.2667|s2cid = 7091307}}</ref> | + | Stimulation of the [[periaqueductal gray]] and [[Periventricular nucleus|periventricular gray]] for [[Pain#Nociceptive|nociceptive pain]], and the [[internal capsule]], [[ventral posterolateral nucleus]], and [[ventral posteromedial nucleus]] for [[Pain#Nociceptive|neuropathic pain]] has produced impressive results with some people, but results vary. One study<ref name = Young>{{cite journal|authors = Young RF & Brechner T|title = Electrical stimulation of the brain for relief of intractable pain due to cancer|journal = Cancer|volume = 57|year = 1986|issue = 6|pages = 1266–72|pmid = 3484665|doi=10.1002/1097-0142(19860315)57:6<1266::aid-cncr2820570634>3.0.co;2-q| doi-access = free}}</ref> of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.<ref name="Johnson">{{cite book|authors = Johnson MI, Oxberry SG & Robb K|chapter = Stimulation-induced analgesia|pages = 235–50|editor = Sykes N, Bennett MI & Yuan C-S|title = Clinical pain management: Cancer pain|edition = 2nd|isbn = 978-0-340-94007-5|publisher = Hodder Arnold|location = London|year = 2008}}</ref> DBS has also been applied for [[phantom limb pain]].<ref name=":23">{{cite journal|vauthors = Kringelbach ML, Jenkinson N, Green AL, Owen SL, Hansen PC, Cornelissen PL, Holliday IE, Stein J, Aziz TZ|title = Deep brain stimulation for chronic pain investigated with magnetoencephalography|journal = NeuroReport|volume = 18|issue = 3|pages = 223–28|date = February 2007|pmid = 17314661|doi = 10.1097/wnr.0b013e328010dc3d|citeseerx = 10.1.1.511.2667|s2cid = 7091307}}</ref> |
Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some people, but results vary. One study of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life. DBS has also been applied for phantom limb pain. | Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some people, but results vary. One study of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life. DBS has also been applied for phantom limb pain. | ||
| − | + | 刺激'''导水管周围灰质( [[periaqueductal gray]])'''和'''脑室周围灰质( [[Periventricular nucleus|periventricular gray]] )'''来治疗'''痛觉性疼痛([[Pain#Nociceptive|nociceptive pain]])''',刺激'''内囊( [[internal capsule]])'''、'''腹侧后外侧核( [[ventral posterolateral nucleus]])'''和'''腹侧后内侧核([[ventral posteromedial nucleus]])'''来治疗'''神经性疼痛([[Pain#Nociceptive|neuropathic pain]])''',对一些人产生了令人印象深刻的结果,但结果各不相同。一项<ref name="Young" /> 针对17名癌症顽固性疼痛患者的研究发现,其中13人几乎没有疼痛,只有4人在干预后出院时需要服用阿片类镇痛药。大多数人最终诉诸于阿片类药物,通常是在生命的最后几周<ref name="Johnson" /> 。DBS也被用于治疗'''幻肢疼痛([[phantom limb pain]])'''<ref name=":23" />。 | |
=== Major depression and obsessive-compulsive disorder === | === Major depression and obsessive-compulsive disorder === | ||
[[File:X-ray of deep brain stimulation in OCD, L.png|thumb|Lateral X-ray of the head: Deep brain stimulation in [[Obsessive–compulsive disorder]] (OCD). 42 year old man, surgery in 2013.|链接=Special:FilePath/X-ray_of_deep_brain_stimulation_in_OCD,_L.png]] | [[File:X-ray of deep brain stimulation in OCD, L.png|thumb|Lateral X-ray of the head: Deep brain stimulation in [[Obsessive–compulsive disorder]] (OCD). 42 year old man, surgery in 2013.|链接=Special:FilePath/X-ray_of_deep_brain_stimulation_in_OCD,_L.png]] | ||
| − | DBS has been used in a small number of clinical trials to treat people with severe [[treatment-resistant depression]] (TRD).<ref name="Anderson">{{cite journal|vauthors = Anderson RJ, Frye MA, Abulseoud OA, Lee KH, McGillivray JA, Berk M, Tye SJ|title = Deep brain stimulation for treatment-resistant depression: efficacy, safety and mechanisms of action|journal = Neuroscience and Biobehavioral Reviews|volume = 36|issue = 8|pages = 1920–33|date = September 2012|pmid = 22721950|doi = 10.1016/j.neubiorev.2012.06.001|s2cid = 207089716}}</ref> A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus,<ref>{{cite journal|vauthors = Accolla EA, Aust S, Merkl A, Schneider GH, Kühn AA, Bajbouj M, Draganski B|title = Deep brain stimulation of the posterior gyrus rectus region for treatment resistant depression|journal = Journal of Affective Disorders|volume = 194|pages = 33–37|date = April 2016|pmid = 26802505|doi = 10.1016/j.jad.2016.01.022|doi-access = free}}</ref> [[nucleus accumbens]],<ref>{{cite journal|vauthors = Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, Joe AY, Kreft M, Lenartz D, Sturm V|title = Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression|journal = Neuropsychopharmacology|volume = 33|issue = 2|pages = 368–77|date = January 2008|pmid = 17429407|doi = 10.1038/sj.npp.1301408|doi-access = free}}</ref> ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula.<ref name="Anderson"/> A recently proposed target of DBS intervention in depression is the superolateral branch of the [[medial forebrain bundle]]; its stimulation lead to surprisingly rapid antidepressant effects.<ref>{{cite journal|vauthors = Schlaepfer TE, Bewernick BH, Kayser S, Mädler B, Coenen VA|title = Rapid effects of deep brain stimulation for treatment-resistant major depression|journal = Biological Psychiatry|volume = 73|issue = 12|pages = 1204–12|date = June 2013|pmid = 23562618|doi = 10.1016/j.biopsych.2013.01.034|s2cid = 6374368}}</ref> | + | DBS has been used in a small number of clinical trials to treat people with severe [[treatment-resistant depression]] (TRD).<ref name="Anderson">{{cite journal|vauthors = Anderson RJ, Frye MA, Abulseoud OA, Lee KH, McGillivray JA, Berk M, Tye SJ|title = Deep brain stimulation for treatment-resistant depression: efficacy, safety and mechanisms of action|journal = Neuroscience and Biobehavioral Reviews|volume = 36|issue = 8|pages = 1920–33|date = September 2012|pmid = 22721950|doi = 10.1016/j.neubiorev.2012.06.001|s2cid = 207089716}}</ref> A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus,<ref name=":24">{{cite journal|vauthors = Accolla EA, Aust S, Merkl A, Schneider GH, Kühn AA, Bajbouj M, Draganski B|title = Deep brain stimulation of the posterior gyrus rectus region for treatment resistant depression|journal = Journal of Affective Disorders|volume = 194|pages = 33–37|date = April 2016|pmid = 26802505|doi = 10.1016/j.jad.2016.01.022|doi-access = free}}</ref> [[nucleus accumbens]],<ref name=":25">{{cite journal|vauthors = Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, Joe AY, Kreft M, Lenartz D, Sturm V|title = Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression|journal = Neuropsychopharmacology|volume = 33|issue = 2|pages = 368–77|date = January 2008|pmid = 17429407|doi = 10.1038/sj.npp.1301408|doi-access = free}}</ref> ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula.<ref name="Anderson"/> A recently proposed target of DBS intervention in depression is the superolateral branch of the [[medial forebrain bundle]]; its stimulation lead to surprisingly rapid antidepressant effects.<ref name=":26">{{cite journal|vauthors = Schlaepfer TE, Bewernick BH, Kayser S, Mädler B, Coenen VA|title = Rapid effects of deep brain stimulation for treatment-resistant major depression|journal = Biological Psychiatry|volume = 73|issue = 12|pages = 1204–12|date = June 2013|pmid = 23562618|doi = 10.1016/j.biopsych.2013.01.034|s2cid = 6374368}}</ref> |
DBS has been used in a small number of clinical trials to treat people with severe treatment-resistant depression (TRD). A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus, nucleus accumbens, ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula. A recently proposed target of DBS intervention in depression is the superolateral branch of the medial forebrain bundle; its stimulation lead to surprisingly rapid antidepressant effects. | DBS has been used in a small number of clinical trials to treat people with severe treatment-resistant depression (TRD). A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus, nucleus accumbens, ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula. A recently proposed target of DBS intervention in depression is the superolateral branch of the medial forebrain bundle; its stimulation lead to surprisingly rapid antidepressant effects. | ||
| − | + | DBS已在少量临床试验中用于治疗严重'''难治性抑郁症([[treatment-resistant depression]])'''(TRD)患者<ref name="Anderson" /> 。DBS治疗TRD的神经解剖学靶点包括膝下扣带回、后直回<ref name=":24" />、伏隔核<ref name=":25" /> 、腹侧囊/腹侧纹状体、丘脑下蒂和外侧缰状核<ref name="Anderson" /> 。最近提出的DBS干预抑郁症的靶点是'''内侧前脑束([[medial forebrain bundle]])'''的上外侧支;它的刺激导致惊人的快速抗抑郁作用<ref name=":26" />。 | |
| − | The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target.<ref name="Anderson"/> Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective [[treatment modality]] in the future.<ref>{{cite journal |last1=Murphy |first1=Destiny N. |last2=Boggio |first2=Paulo |last3=Fregni |first3=Felipe |title=Transcranial direct current stimulation as a therapeutic tool for the treatment of major depression: insights from past and recent clinical studies |journal=Curr Opin Psychiatry |year=2009 |volume=22 |issue=3 |pages=306–11 |doi=10.1097/YCO.0b013e32832a133f |pmid=19339889 |s2cid=11392351}}</ref> In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment.<ref name="Delgado 1986">{{cite book|last=Delgado|first=Jose|title=Physical Control of the Mind: Toward a Psychocivilized Society|year=1986|publisher=Harper and Row|location=New York |isbn=0-06-131914-7}}</ref><ref name="Faria 3">{{cite journal|vauthors = Faria MA|title = Violence, mental illness, and the brain – A brief history of psychosurgery: Part 3 – From deep brain stimulation to amygdalotomy for violent behavior, seizures, and pathological aggression in humans|journal = Surgical Neurology International|volume = 4|issue = 1|pages = 91|year = 2013|pmid = 23956934|pmc = 3740620|doi = 10.4103/2152-7806.115162}}</ref><ref>{{cite journal|vauthors = Robison RA, Taghva A, Liu CY, Apuzzo ML|title = Surgery of the mind, mood, and conscious state: an idea in evolution|journal = World Neurosurgery|volume = 77|issue = 5–6|pages = 662–86|year = 2012|pmid = 22446082|doi = 10.1016/j.wneu.2012.03.005}}</ref> | + | The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target.<ref name="Anderson"/> Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective [[treatment modality]] in the future.<ref name=":27">{{cite journal |last1=Murphy |first1=Destiny N. |last2=Boggio |first2=Paulo |last3=Fregni |first3=Felipe |title=Transcranial direct current stimulation as a therapeutic tool for the treatment of major depression: insights from past and recent clinical studies |journal=Curr Opin Psychiatry |year=2009 |volume=22 |issue=3 |pages=306–11 |doi=10.1097/YCO.0b013e32832a133f |pmid=19339889 |s2cid=11392351}}</ref> In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment.<ref name="Delgado 1986">{{cite book|last=Delgado|first=Jose|title=Physical Control of the Mind: Toward a Psychocivilized Society|year=1986|publisher=Harper and Row|location=New York |isbn=0-06-131914-7}}</ref><ref name="Faria 3">{{cite journal|vauthors = Faria MA|title = Violence, mental illness, and the brain – A brief history of psychosurgery: Part 3 – From deep brain stimulation to amygdalotomy for violent behavior, seizures, and pathological aggression in humans|journal = Surgical Neurology International|volume = 4|issue = 1|pages = 91|year = 2013|pmid = 23956934|pmc = 3740620|doi = 10.4103/2152-7806.115162}}</ref><ref name=":28">{{cite journal|vauthors = Robison RA, Taghva A, Liu CY, Apuzzo ML|title = Surgery of the mind, mood, and conscious state: an idea in evolution|journal = World Neurosurgery|volume = 77|issue = 5–6|pages = 662–86|year = 2012|pmid = 22446082|doi = 10.1016/j.wneu.2012.03.005}}</ref> |
The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target. Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective treatment modality in the future. In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment. | The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target. Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective treatment modality in the future. In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment. | ||
| − | + | DBS治疗TRD的早期试验数量较少,目前限制了最佳神经解剖学靶点的选择<ref name="Anderson" /> 。证据不足以支持DBS作为抑郁症的治疗方式;然而,该手术可能是未来一种有效的治疗方式([[treatment modality]])<ref name=":27" />。事实上,神经外科文献中已经记录了有益的结果,包括一些为重度抑郁的人提供便携式刺激器进行自我治疗的例子<ref name="Delgado 1986" /><ref name="Faria 3" /><ref name=":28" />。 | |
| − | A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders.<ref name=Lakhan>{{cite journal|vauthors = Lakhan SE, Callaway E|title = Deep brain stimulation for obsessive-compulsive disorder and treatment-resistant depression: systematic review|journal = BMC Research Notes|volume = 3|issue = 1|pages = 60|date = March 2010|pmid = 20202203|pmc = 2838907|doi = 10.1186/1756-0500-3-60}}</ref> The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study.<ref>{{cite journal|vauthors = Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O'Reardon JP, Eskandar EN, Baltuch GH, Machado AD, Kondziolka D, Cusin C, Evans KC, Price LH, Jacobs K, Pandya M, Denko T, Tyrka AR, Brelje T, Deckersbach T, Kubu C, Malone DA|title = A Randomized Sham-Controlled Trial of Deep Brain Stimulation of the Ventral Capsule/Ventral Striatum for Chronic Treatment-Resistant Depression|journal = Biological Psychiatry|volume = 78|issue = 4|pages = 240–48|date = August 2015|pmid = 25726497|doi = 10.1016/j.biopsych.2014.11.023|s2cid = 22644265}}</ref> However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders).<ref>{{cite journal|vauthors = Bergfeld IO, Mantione M, Hoogendoorn ML, Ruhé HG, Notten P, van Laarhoven J, Visser I, Figee M, de Kwaasteniet BP, Horst F, Schene AH, van den Munckhof P, Beute G, Schuurman R, Denys D|display-authors = 6|title = Deep Brain Stimulation of the Ventral Anterior Limb of the Internal Capsule for Treatment-Resistant Depression: A Randomized Clinical Trial|journal = JAMA Psychiatry|volume = 73|issue = 5|pages = 456–64|date = May 2016|pmid = 27049915|doi = 10.1001/jamapsychiatry.2016.0152|doi-access = free}}</ref> Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients.<ref>{{cite journal|vauthors = Alonso P, Cuadras D, Gabriëls L, Denys D, Goodman W, Greenberg BD, Jimenez-Ponce F, Kuhn J, Lenartz D, Mallet L, Nuttin B, Real E, Segalas C, Schuurman R, du Montcel ST, Menchon JM|display-authors = 6|title = Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Meta-Analysis of Treatment Outcome and Predictors of Response|journal = PLOS ONE|volume = 10|issue = 7|pages = e0133591|date = 2015-07-24|pmid = 26208305|pmc = 4514753|doi = 10.1371/journal.pone.0133591|bibcode = 2015PLoSO..1033591A|doi-access = free}}</ref> Based on these results the [[Food and Drug Administration]] (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so. | + | A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders.<ref name=Lakhan>{{cite journal|vauthors = Lakhan SE, Callaway E|title = Deep brain stimulation for obsessive-compulsive disorder and treatment-resistant depression: systematic review|journal = BMC Research Notes|volume = 3|issue = 1|pages = 60|date = March 2010|pmid = 20202203|pmc = 2838907|doi = 10.1186/1756-0500-3-60}}</ref> The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study.<ref name=":29">{{cite journal|vauthors = Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O'Reardon JP, Eskandar EN, Baltuch GH, Machado AD, Kondziolka D, Cusin C, Evans KC, Price LH, Jacobs K, Pandya M, Denko T, Tyrka AR, Brelje T, Deckersbach T, Kubu C, Malone DA|title = A Randomized Sham-Controlled Trial of Deep Brain Stimulation of the Ventral Capsule/Ventral Striatum for Chronic Treatment-Resistant Depression|journal = Biological Psychiatry|volume = 78|issue = 4|pages = 240–48|date = August 2015|pmid = 25726497|doi = 10.1016/j.biopsych.2014.11.023|s2cid = 22644265}}</ref> However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders).<ref name=":30">{{cite journal|vauthors = Bergfeld IO, Mantione M, Hoogendoorn ML, Ruhé HG, Notten P, van Laarhoven J, Visser I, Figee M, de Kwaasteniet BP, Horst F, Schene AH, van den Munckhof P, Beute G, Schuurman R, Denys D|display-authors = 6|title = Deep Brain Stimulation of the Ventral Anterior Limb of the Internal Capsule for Treatment-Resistant Depression: A Randomized Clinical Trial|journal = JAMA Psychiatry|volume = 73|issue = 5|pages = 456–64|date = May 2016|pmid = 27049915|doi = 10.1001/jamapsychiatry.2016.0152|doi-access = free}}</ref> Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients.<ref name=":31">{{cite journal|vauthors = Alonso P, Cuadras D, Gabriëls L, Denys D, Goodman W, Greenberg BD, Jimenez-Ponce F, Kuhn J, Lenartz D, Mallet L, Nuttin B, Real E, Segalas C, Schuurman R, du Montcel ST, Menchon JM|display-authors = 6|title = Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Meta-Analysis of Treatment Outcome and Predictors of Response|journal = PLOS ONE|volume = 10|issue = 7|pages = e0133591|date = 2015-07-24|pmid = 26208305|pmc = 4514753|doi = 10.1371/journal.pone.0133591|bibcode = 2015PLoSO..1033591A|doi-access = free}}</ref> Based on these results the [[Food and Drug Administration]] (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so. |
A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders. The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study. However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders). Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients. Based on these results the Food and Drug Administration (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so. | A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders. The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study. However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders). Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients. Based on these results the Food and Drug Administration (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so. | ||
| − | + | 一项针对TRD和OCD的系统回顾发现了23例DBS, 9例为OCD, 7例为TRD, 1例为两者。“大约一半的患者确实表现出了显著的改善”,而且考虑到精神病患者的年龄相对于运动障碍患者的年龄,不良事件“通常微不足道”<ref name="Lakhan" /> 。在第一个随机对照研究中,DBS用于治疗以腹侧囊/腹侧纹状体区域为靶点的TRD,在16周的研究结束时,active组和sham组之间的缓解率没有显著差异<ref name=":29" />。然而,另一项腹侧胶囊DBS治疗TRD的随机对照研究确实表明,有效DBS(有效率为44%)和假DBS(有效率为0%)的缓解率存在显著差异)<ref name=":30" /> 。DBS治疗强迫症疗效显著,重症和难治性患者平均有效率为60%<ref name=":31" />。根据这些结果,美国'''食品和药物管理局([[Food and Drug Administration]] )'''(FDA)根据人道主义器械豁免(HDE)批准了DBS治疗顽症,要求只有在有专业资格的医院才能实施该手术。 | |
DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality".<ref name=Moreines>{{cite journal|vauthors = Moreines JL, McClintock SM, Holtzheimer PE|title = Neuropsychologic effects of neuromodulation techniques for treatment-resistant depression: a review|journal = Brain Stimulation|volume = 4|issue = 1|pages = 17–27|date = January 2011|pmid = 21255751|pmc = 3023999|doi = 10.1016/j.brs.2010.01.005}}</ref> | DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality".<ref name=Moreines>{{cite journal|vauthors = Moreines JL, McClintock SM, Holtzheimer PE|title = Neuropsychologic effects of neuromodulation techniques for treatment-resistant depression: a review|journal = Brain Stimulation|volume = 4|issue = 1|pages = 17–27|date = January 2011|pmid = 21255751|pmc = 3023999|doi = 10.1016/j.brs.2010.01.005}}</ref> | ||
| 第208行: | 第208行: | ||
DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality". | DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality". | ||
| − | + | DBS治疗TRD与抗抑郁药一样有效,有良好的反应率和缓解率,但不良反应和安全性必须得到更全面的评估。常见的副作用包括“伤口感染、围手术期头痛、情绪恶化/烦躁以及自杀倾向增加”<ref name="Moreines" />。 | |
=== Other clinical applications === | === Other clinical applications === | ||
| − | Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases.<ref>{{cite journal|vauthors = Krauss JK|title = Deep brain stimulation for dystonia in adults. Overview and developments|journal = Stereotactic and Functional Neurosurgery|volume = 78|issue = 3–4|pages = 168–82|year = 2002|pmid = 12652041|doi = 10.1159/000068963|s2cid = 71888143}}</ref> The procedure has been tested for effectiveness in people with [[epilepsy]] that is resistant to medication.<ref>{{cite journal|vauthors = Wu C, Sharan AD|title = Neurostimulation for the treatment of epilepsy: a review of current surgical interventions|journal = Neuromodulation|volume = 16|issue = 1|pages = 10–24; discussion 24|date = Jan–Feb 2013|pmid = 22947069|doi = 10.1111/j.1525-1403.2012.00501.x|s2cid = 1711587}}</ref> DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.{{citation needed|date=January 2017}} | + | Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases.<ref name=":32">{{cite journal|vauthors = Krauss JK|title = Deep brain stimulation for dystonia in adults. Overview and developments|journal = Stereotactic and Functional Neurosurgery|volume = 78|issue = 3–4|pages = 168–82|year = 2002|pmid = 12652041|doi = 10.1159/000068963|s2cid = 71888143}}</ref> The procedure has been tested for effectiveness in people with [[epilepsy]] that is resistant to medication.<ref name=":33">{{cite journal|vauthors = Wu C, Sharan AD|title = Neurostimulation for the treatment of epilepsy: a review of current surgical interventions|journal = Neuromodulation|volume = 16|issue = 1|pages = 10–24; discussion 24|date = Jan–Feb 2013|pmid = 22947069|doi = 10.1111/j.1525-1403.2012.00501.x|s2cid = 1711587}}</ref> DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.{{citation needed|date=January 2017}} |
Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases. The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication. DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation. | Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases. The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication. DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation. | ||
| − | + | DBS对肌张力障碍患者的治疗结果显示,积极效果往往在数周至数月的时间内逐渐显现,至少在某些情况下显示出功能重组的作用<ref name=":32" /> 。该方法已经在对药物有抗药性的'''癫痫([[epilepsy]])'''患者身上进行了有效性测试<ref name=":33" /> 。DBS可通过程序性或反应性刺激减少或消除癫痫发作.{{citation needed|date=January 2017}}。 | |
DBS of the [[Septal nuclei|septal areas]] of persons with [[schizophrenia]] have resulted in enhanced alertness, cooperation, and euphoria.<ref>{{cite journal|vauthors = Heath RG|title = Pleasure and brain activity in man. Deep and surface electroencephalograms during orgasm|journal = The Journal of Nervous and Mental Disease|volume = 154|issue = 1|pages = 3–18|date = January 1972|pmid = 5007439|doi = 10.1097/00005053-197201000-00002|s2cid = 136706}}</ref> Persons with [[narcolepsy]] and [[complex-partial seizures]] also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.<ref name="Faria 3" /> | DBS of the [[Septal nuclei|septal areas]] of persons with [[schizophrenia]] have resulted in enhanced alertness, cooperation, and euphoria.<ref>{{cite journal|vauthors = Heath RG|title = Pleasure and brain activity in man. Deep and surface electroencephalograms during orgasm|journal = The Journal of Nervous and Mental Disease|volume = 154|issue = 1|pages = 3–18|date = January 1972|pmid = 5007439|doi = 10.1097/00005053-197201000-00002|s2cid = 136706}}</ref> Persons with [[narcolepsy]] and [[complex-partial seizures]] also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.<ref name="Faria 3" /> | ||
| 第221行: | 第221行: | ||
DBS of the septal areas of persons with schizophrenia have resulted in enhanced alertness, cooperation, and euphoria. Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei. | DBS of the septal areas of persons with schizophrenia have resulted in enhanced alertness, cooperation, and euphoria. Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei. | ||
| − | + | 对'''精神分裂症患者([[schizophrenia]])'''的'''鼻中隔区域([[Septal nuclei|septal areas]])'''进行DBS可增强警惕性、合作性和欣快感<ref name=":32" /> 。有'''嗜睡症([[narcolepsy]] )'''和'''复杂部分性癫痫([[complex-partial seizures]])'''的患者也报告说,自我诱发的间隔核深部脑刺激能产生欣快感和性想法<ref name="Faria 3" />。 | |
| − | Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left [[hippocampus]] at 3mA, and the right [[hippocampus]] at 1 mA.<ref>{{cite journal|vauthors = Surbeck W, Bouthillier A, Nguyen DK|title = Bilateral cortical representation of orgasmic ecstasy localized by depth electrodes|journal = Epilepsy & Behavior Case Reports|volume = 1|pages = 62–65|pmid = 25667829|pmc = 4150648|doi = 10.1016/j.ebcr.2013.03.002|year = 2013}}</ref> | + | Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left [[hippocampus]] at 3mA, and the right [[hippocampus]] at 1 mA.<ref name=":34">{{cite journal|vauthors = Surbeck W, Bouthillier A, Nguyen DK|title = Bilateral cortical representation of orgasmic ecstasy localized by depth electrodes|journal = Epilepsy & Behavior Case Reports|volume = 1|pages = 62–65|pmid = 25667829|pmc = 4150648|doi = 10.1016/j.ebcr.2013.03.002|year = 2013}}</ref> |
Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA. | Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA. | ||
| − | + | 据报道,通过深度电极对大脑进行电刺激,左侧'''海马体( [[hippocampus]] )'''为3毫安,右侧'''海马体([[hippocampus]])'''为1毫安<ref name=":34" />。 | |
| − | In 2015, a group of Brazilian researchers led by neurosurgeon {{ill|Erich Fonoff|pt|Erich Fonoff}} described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.<ref>{{cite journal|vauthors = Fonoff ET, Azevedo A, Angelos JS, Martinez RC, Navarro J, Reis PR, Sepulveda ME, Cury RG, Ghilardi MG, Teixeira MJ, Lopez WO|title = Simultaneous bilateral stereotactic procedure for deep brain stimulation implants: a significant step for reducing operation time|journal = Journal of Neurosurgery|volume = 125|issue = 1|pages = 85–89|date = July 2016|pmid = 26684776|doi = 10.3171/2015.7.JNS151026|doi-access = free}}</ref> | + | In 2015, a group of Brazilian researchers led by neurosurgeon {{ill|Erich Fonoff|pt|Erich Fonoff}} described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.<ref name=":35">{{cite journal|vauthors = Fonoff ET, Azevedo A, Angelos JS, Martinez RC, Navarro J, Reis PR, Sepulveda ME, Cury RG, Ghilardi MG, Teixeira MJ, Lopez WO|title = Simultaneous bilateral stereotactic procedure for deep brain stimulation implants: a significant step for reducing operation time|journal = Journal of Neurosurgery|volume = 125|issue = 1|pages = 85–89|date = July 2016|pmid = 26684776|doi = 10.3171/2015.7.JNS151026|doi-access = free}}</ref> |
In 2015, a group of Brazilian researchers led by neurosurgeon described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy. | In 2015, a group of Brazilian researchers led by neurosurgeon described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy. | ||
| − | + | 2015年,由神经外科医生领导的一组巴西研究人员描述了一种新技术,该技术允许同时植入电极,称为双侧立体定向术。主要的好处是花在手术上的时间更少,准确性更高<ref name=":35" />。 | |
| − | In 2016, DBS was found to improve learning and memory in a mouse model of [[Rett syndrome]].<ref>{{cite journal|vauthors = Lu H, Ash RT, He L, Kee SE, Wang W, Yu D, Hao S, Meng X, Ure K, Ito-Ishida A, Tang B, Sun Y, Ji D, Tang J, Arenkiel BR, Smirnakis SM, Zoghbi HY|title = Loss and Gain of MeCP2 Cause Similar Hippocampal Circuit Dysfunction that Is Rescued by Deep Brain Stimulation in a Rett Syndrome Mouse Model|journal = Neuron|volume = 91|issue = 4|pages = 739–47|date = August 2016|pmid = 27499081|pmc = 5019177|doi = 10.1016/j.neuron.2016.07.018}}</ref> More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis,<ref>{{cite journal|vauthors = Pohodich AE, Yalamanchili H, Raman AT, Wan YW, Gundry M, Hao S, Jin H, Tang J, Liu Z, Zoghbi HY|title = Forniceal deep brain stimulation induces gene expression and splicing changes that promote neurogenesis and plasticity|journal = eLife|volume = 7|date = March 2018|pmid = 29570050|pmc = 5906096|doi = 10.7554/elife.34031}}</ref> making some first steps at explaining the restoration of hippocampal circuit function. | + | In 2016, DBS was found to improve learning and memory in a mouse model of [[Rett syndrome]].<ref name=":36">{{cite journal|vauthors = Lu H, Ash RT, He L, Kee SE, Wang W, Yu D, Hao S, Meng X, Ure K, Ito-Ishida A, Tang B, Sun Y, Ji D, Tang J, Arenkiel BR, Smirnakis SM, Zoghbi HY|title = Loss and Gain of MeCP2 Cause Similar Hippocampal Circuit Dysfunction that Is Rescued by Deep Brain Stimulation in a Rett Syndrome Mouse Model|journal = Neuron|volume = 91|issue = 4|pages = 739–47|date = August 2016|pmid = 27499081|pmc = 5019177|doi = 10.1016/j.neuron.2016.07.018}}</ref> More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis,<ref name=":37">{{cite journal|vauthors = Pohodich AE, Yalamanchili H, Raman AT, Wan YW, Gundry M, Hao S, Jin H, Tang J, Liu Z, Zoghbi HY|title = Forniceal deep brain stimulation induces gene expression and splicing changes that promote neurogenesis and plasticity|journal = eLife|volume = 7|date = March 2018|pmid = 29570050|pmc = 5906096|doi = 10.7554/elife.34031}}</ref> making some first steps at explaining the restoration of hippocampal circuit function. |
In 2016, DBS was found to improve learning and memory in a mouse model of Rett syndrome. More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis, making some first steps at explaining the restoration of hippocampal circuit function. | In 2016, DBS was found to improve learning and memory in a mouse model of Rett syndrome. More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis, making some first steps at explaining the restoration of hippocampal circuit function. | ||
| − | + | 2016年,DBS被发现可以改善'''Rett综合征([[Rett syndrome]])'''小鼠模型的学习和记忆<ref name=":36" /> 。最近2018年的研究表明,穹穴DBS上调了涉及突触功能、细胞存活和神经发生的基因<ref name=":37" /> ,在解释海马回路功能的恢复方面迈出了一些第一步。 | |
== See also == | == See also == | ||
2022年7月7日 (四) 15:55的版本
此词条由神经动力学读书会词条梳理志愿者苏苏Anny翻译审校,未经专家审核,带来阅读不便,请见谅。
此词条暂由彩云小译翻译,翻译字数共2470,未经人工整理和审校,带来阅读不便,请见谅。
模板:Infobox medical intervention
Deep brain stimulation (DBS) is a neurosurgical procedure involving the placement of a medical device called a neurostimulator, which sends electrical impulses, through implanted electrodes, to specific targets in the brain (the brain nucleus) for the treatment of movement disorders, including Parkinson's disease, essential tremor, dystonia,[1] and other conditions such as obsessive-compulsive disorder (OCD) and epilepsy. While its underlying principles and mechanisms are not fully understood, DBS directly changes brain activity in a controlled manner.[2][3]
Deep brain stimulation (DBS) is a neurosurgical procedure involving the placement of a medical device called a neurostimulator, which sends electrical impulses, through implanted electrodes, to specific targets in the brain (the brain nucleus) for the treatment of movement disorders, including Parkinson's disease, essential tremor, dystonia, and other conditions such as obsessive-compulsive disorder (OCD) and epilepsy. While its underlying principles and mechanisms are not fully understood, DBS directly changes brain activity in a controlled manner.
脑深部电刺激(DBS)是神经外科手术(neurosurgical)中的操作之一,包括放置一种叫做神经刺激器( neurostimulator)的医疗设备,通过植入的电极(electrode)将电脉冲发送到大脑(brain)中的特定目标(脑核(brain nucleus)) ,治疗包括帕金森病(Parkinson's disease)、原发性震颤(essential tremor)、肌张力障碍(dystonia)[1]和其他疾病,如强迫症(obsessive-compulsive disorder)和癫痫(epilepsy),引起的运动障碍。虽然其基本原理和机制尚不完全清楚,DBS 是一种可控的直接改变大脑活动的方式.[2][3]。
DBS has been approved by the Food and Drug Administration as a treatment for essential tremor and Parkinson's disease (PD) since 1997.[4] DBS was approved for dystonia in 2003,[5] Obsessive–compulsive disorder (OCD) in 2009, and epilepsy in 2018.[6][7][8] DBS has been studied in clinical trials as a potential treatment for chronic pain for various affective disorders, including major depression. It is one of few neurosurgical procedures that allow blinded studies.[1]
DBS has been approved by the Food and Drug Administration as a treatment for essential tremor and Parkinson's disease (PD) since 1997. DBS was approved for dystonia in 2003,'Brain pacemaker' treats dystonia. KNBC TV, April 22, 2003. Retrieved October 18, 2006. Obsessive–compulsive disorder (OCD) in 2009, and epilepsy in 2018. DBS has been studied in clinical trials as a potential treatment for chronic pain for various affective disorders, including major depression. It is one of few neurosurgical procedures that allow blinded studies.
1997年,DBS 已经被美国食品和药物管理局(Food and Drug Administration)批准用于治疗原发性震颤和帕金森病(Parkinson's disease)[4]。2003年被批准,以“脑起搏器”的方法用于肌张力障碍(dystonia)[5] ,2009年被批准用于强迫症,2018年用于癫痫[6][7][8]。DBS 已经在临床试验中被研究用作各种情感障碍(包括重度抑郁症(major depression))的慢性疼痛(chronic pain)的潜在治疗方法。这是少数允许盲法研究( blinded studies)的神经外科手术之一[1]。
Medical use

Parkinson's disease
DBS is used to manage some of the symptoms of Parkinson's disease that cannot be adequately controlled with medications.[9][10] PD is treated by applying high-frequency (> 100 Hz) stimulation to three target structures namely to entrolateral thalamus, internal pallidum, and subthalamic nucleus (STN) to mimic the clinical effects of lesioning.[11] It is recommended for people who have PD with motor fluctuations and tremor inadequately controlled by medication, or to those who are intolerant to medication, as long as they do not have severe neuropsychiatric problems.[12] Four areas of the brain have been treated with neural stimulators in PD. These are the globus pallidus internus, thalamus, subthalamic nucleus and the pedunculopontine nucleus. However, most DBS surgeries in routine practice target either the globus pallidus internus, or the Subthalamic nucleus.
- DBS of the globus pallidus internus reduces uncontrollable shaking movements called dyskinesias. This enables a patient to take adequate quantities of medications (especially levodopa), thus leading to better control of symptoms.
- DBS of the subthalamic nucleus directly reduces symptoms of Parkinson's. This enables a decrease in the dose of anti-parkinsonian medications.
- DBS of the PPN may help with freezing of gait, while DBS of the thalamus may help with tremor. These targets are not routinely utilized.
DBS is used to manage some of the symptoms of Parkinson's disease that cannot be adequately controlled with medications.U.S. Department of Health and Human Services. FDA approves implanted brain stimulator to control tremors. Retrieved February 10, 2015. PD is treated by applying high-frequency (> 100 Hz) stimulation to three target structures namely to entrolateral thalamus, internal pallidum, and subthalamic nucleus (STN) to mimic the clinical effects of lesioning.Koller, W. and Melamed, E., 2007. Parkinson's disease and related disorders. 1st ed. Edinburgh: Elsevier. It is recommended for people who have PD with motor fluctuations and tremor inadequately controlled by medication, or to those who are intolerant to medication, as long as they do not have severe neuropsychiatric problems. Four areas of the brain have been treated with neural stimulators in PD. These are the globus pallidus internus, thalamus, subthalamic nucleus and the pedunculopontine nucleus. However, most DBS surgeries in routine practice target either the globus pallidus internus, or the Subthalamic nucleus.
- DBS of the globus pallidus internus reduces uncontrollable shaking movements called dyskinesias. This enables a patient to take adequate quantities of medications (especially levodopa), thus leading to better control of symptoms.
- DBS of the subthalamic nucleus directly reduces symptoms of Parkinson's. This enables a decrease in the dose of anti-parkinsonian medications.
- DBS of the PPN may help with freezing of gait, while DBS of the thalamus may help with tremor. These targets are not routinely utilized.
DBS用于治疗帕金森病的一些无法用药完全控制的症状.[9][10] 。通过对丘脑内外侧、内苍白球和丘脑下核(STN)三个靶结构应用高频(> 100 Hz)刺激治疗PD,以模拟病变的临床效果[11] 。它适合推荐给药物控制不充分的运动波动和震颤的PD患者,或对药物不耐受的患者,只要他们没有严重的神经精神问题[12] 。在帕金森病中,有苍白球内( globus pallidus internus)、丘脑( thalamus)、丘脑下核(subthalamic nucleus)和桥脚核(pedunculopontine nucleus)四个脑区使用神经刺激器进行治疗。然而,在常规手术中,大多数DBS手术不是针对苍白球内,就是针对丘脑下核。
- 苍白球内的DBS减少了不可控的震颤运动,称为运动障碍(dyskinesias)。这使患者能够服用足够数量的药物(特别是左旋多巴),从而更好地控制症状。
- 丘脑底核深部脑刺激可直接减轻帕金森病症状。这可以减少抗帕金森药物的剂量。
- PPN的DBS可能有助于步态冻结,而丘脑的DBS可能有助于颤抖。这些靶标通常不被使用。
Selection of the correct DBS target is a complicated process. Multiple clinical characteristics are used to select the target including – identifying the most troublesome symptoms, the dose of levodopa that the patient is currently taking, the effects and side-effects of current medications and concurrent problems. For example, subthalamic nucleus DBS may worsen depression and hence is not preferred in patients with uncontrolled depression.
Selection of the correct DBS target is a complicated process. Multiple clinical characteristics are used to select the target including – identifying the most troublesome symptoms, the dose of levodopa that the patient is currently taking, the effects and side-effects of current medications and concurrent problems. For example, subthalamic nucleus DBS may worsen depression and hence is not preferred in patients with uncontrolled depression.
选择正确的 DBS 目标是一个复杂的过程。多种临床特征被用来选择目标,包括识别最棘手的症状、患者目前正在服用的左旋多巴的剂量、当前药物的作用和副作用以及同时出现的问题。例如,丘脑下核 DBS 可能会加重抑郁症,因此对于无法控制的抑郁症患者来说并不是首选。
Generally DBS is associated with 30–60% improvement in motor score evaluations.[13]
Generally DBS is associated with 30–60% improvement in motor score evaluations.
一般来说,DBS 与运动成绩评定的30-60% 的改善有关[13]。
Tourette syndrome
DBS has been used experimentally in treating adults with severe Tourette syndrome who do not respond to conventional treatment. Despite widely publicized early successes, DBS remains a highly experimental procedure for the treatment of Tourette's, and more study is needed to determine whether long-term benefits outweigh the risks.[14][15][16][17] The procedure is well tolerated, but complications include "short battery life, abrupt symptom worsening upon cessation of stimulation, hypomanic or manic conversion, and the significant time and effort involved in optimizing stimulation parameters".[18] As of 2006, five people with TS had been reported on; all experienced reduction in tics and the disappearance of obsessive-compulsive behaviors.[18]
DBS has been used experimentally in treating adults with severe Tourette syndrome who do not respond to conventional treatment. Despite widely publicized early successes, DBS remains a highly experimental procedure for the treatment of Tourette's, and more study is needed to determine whether long-term benefits outweigh the risks. Also see Tourette Syndrome Association. Statement: Deep Brain Stimulation and Tourette Syndrome. Retrieved November 22, 2005. The procedure is well tolerated, but complications include "short battery life, abrupt symptom worsening upon cessation of stimulation, hypomanic or manic conversion, and the significant time and effort involved in optimizing stimulation parameters". As of 2006, five people with TS had been reported on; all experienced reduction in tics and the disappearance of obsessive-compulsive behaviors.
DBS已被实验性地用于治疗对常规治疗没有反应的成人严重图雷特综合征( Tourette syndrome)。尽管早期的成功被广泛宣传,DBS治疗图雷特氏症仍然是一个高度实验性(experimental )的程序,需要更多的研究来确定长期的好处是否大于风险[14][15][16][17] 。该手术耐受性良好,但并发症包括“电池寿命短,停止刺激后症状突然恶化,轻度躁狂或躁狂转化,以及优化刺激参数所需的大量时间和精力”[18] 。截至2006年,有5人被报告患有TS;所有人都经历了抽搐的减少和强迫行为的消失[18]。
The procedure is invasive and expensive, and requires long-term expert care. Benefits for severe Tourette's are not conclusive, considering less robust effects of this surgery seen in the Netherlands. Tourette's is more common in pediatric populations, tending to remit in adulthood, so in general this would not be a recommended procedure for use on children. Because diagnosis of Tourette's is made based on a history of symptoms rather than analysis of neurological activity, it may not always be clear how to apply DBS for a particular person. Due to concern over the use of DBS in Tourette syndrome treatment, the Tourette Association of America convened a group of experts to develop recommendations guiding the use and potential clinical trials of DBS for TS.[19]
The procedure is invasive and expensive, and requires long-term expert care. Benefits for severe Tourette's are not conclusive, considering less robust effects of this surgery seen in the Netherlands. Tourette's is more common in pediatric populations, tending to remit in adulthood, so in general this would not be a recommended procedure for use on children. Because diagnosis of Tourette's is made based on a history of symptoms rather than analysis of neurological activity, it may not always be clear how to apply DBS for a particular person. Due to concern over the use of DBS in Tourette syndrome treatment, the Tourette Association of America convened a group of experts to develop recommendations guiding the use and potential clinical trials of DBS for TS.
这种手术具有侵入性,费用昂贵,需要长期的专家护理。考虑到在荷兰( Netherlands)进行的这种手术效果较差,重度抽动秽语综合症的益处还不能下结论。抽动秽语综合症在儿童群体中更为常见,成年后趋于缓解,所以一般不推荐在儿童身上使用这种疗法。因为抽动秽语综合症的诊断是基于症状的历史而不是神经活动的分析,所以如何为特定的人应用 DBS 并不总是很清楚。由于担心使用DBS治疗抽动秽语综合症(Tourette syndrome treatment),美国图雷特协会( Tourette Association of America)召集了一组专家来制定建议,指导DBS治疗TS的使用和潜在的临床试验(clinical trials)[19]。
Robertson reported that DBS had been used on 55 adults by 2011, remained an experimental treatment at that time, and recommended that the procedure "should only be conducted by experienced functional neurosurgeons operating in centres which also have a dedicated Tourette syndrome clinic".[15] According to Malone et al. (2006), "Only patients with severe, debilitating, and treatment-refractory illness should be considered; while those with severe personality disorders and substance-abuse problems should be excluded."[18] Du et al. (2010) say, "As an invasive therapy, DBS is currently only advisable for severely affected, treatment-refractory TS adults".[16] Singer (2011) says, "pending determination of patient selection criteria and the outcome of carefully controlled clinical trials, a cautious approach is recommended".[14] Viswanathan et al. (2012) say DBS should be used for people with "severe functional impairment that cannot be managed medically".[20]
Robertson reported that DBS had been used on 55 adults by 2011, remained an experimental treatment at that time, and recommended that the procedure "should only be conducted by experienced functional neurosurgeons operating in centres which also have a dedicated Tourette syndrome clinic". According to Malone et al. (2006), "Only patients with severe, debilitating, and treatment-refractory illness should be considered; while those with severe personality disorders and substance-abuse problems should be excluded." Du et al. (2010) say, "As an invasive therapy, DBS is currently only advisable for severely affected, treatment-refractory TS adults". Singer (2011) says, "pending determination of patient selection criteria and the outcome of carefully controlled clinical trials, a cautious approach is recommended". Viswanathan et al. (2012) say DBS should be used for people with "severe functional impairment that cannot be managed medically".
Robertson 报告说,截至2011年,DBS 已经在55名成年人身上使用,在当时仍然是一种试验性的治疗方法,并且建议这种手术“应该只由有经验的功能性神经外科医生进行,这些医生所在的中心还有一个专门的图雷特氏综合症诊所”[15] 。根据Malone等人的说法(2006年) ,“只有患有严重的、使人衰弱的和治疗难以治愈的疾病的患者才应该被考虑; 而那些有严重的人格障碍和物质滥用问题的患者应该被排除在外“"[18]。Du 等人(2010)说,“作为一种侵入性治疗,DBS 目前仅适用于严重受影响、治疗难治性 TS 的成年人”[16] 。Singer (2011年)说,“在确定患者选择标准和仔细控制的临床试验结果之前,建议采取谨慎的方法”[14]。Viswanathan等人(2012)表示,DBS 应该用于“严重功能障碍且无法医学治疗”的患者。
Adverse effects
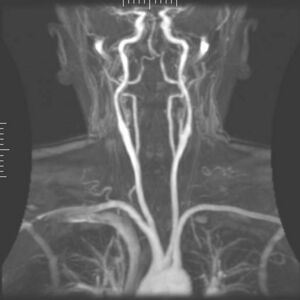
thumb|left|Arteriogram of the arterial supply that can hemorrhage during DBS implantation.
拇指|左| DBS植入时可出血的动脉供应动脉造影。
DBS carries the risks of major surgery, with a complication rate related to the experience of the surgical team. The major complications include hemorrhage (1–2%) and infection (3–5%).[21]
DBS carries the risks of major surgery, with a complication rate related to the experience of the surgical team. The major complications include hemorrhage (1–2%) and infection (3–5%).
DBS具有大手术的风险,并发症的发生率与手术团队的经验有关。主要并发症包括出血(1-2%)和感染(3-5%)[21]。
The potential exists for neuropsychiatric side effects after DBS, including apathy, hallucinations, hypersexuality, cognitive dysfunction, depression, and euphoria. However, these effects may be temporary and related to (1) correct placement of electrodes, (2) open-loop VS closed loop stimulation , meaning a constant stimulation or an A.I. monitoring delivery system[22] and (3) calibration of the stimulator, so these side effects are potentially reversible.[23]
The potential exists for neuropsychiatric side effects after DBS, including apathy, hallucinations, hypersexuality, cognitive dysfunction, depression, and euphoria. However, these effects may be temporary and related to (1) correct placement of electrodes, (2) open-loop VS closed loop stimulation , meaning a constant stimulation or an A.I. monitoring delivery system and (3) calibration of the stimulator, so these side effects are potentially reversible.
DBS 有可能导致神经精神(neuropsychiatric)方面的副作用,包括冷漠(apathy)、幻觉(hallucinations)、性欲亢进(hypersexuality)、认知功能障碍(cognitive dysfunction)、抑郁(depression)和欣快感(euphoria)。然而,这些影响可能是暂时的,与(1)电极的正确放置,(2)开环VS闭环刺激,意味着持续刺激或人工智能监测传输系统[22] ,以及(3)刺激器的校准有关,因此这些副作用可能是可逆的[23]。
Because the brain can shift slightly during surgery, the electrodes can become displaced or dislodged from the specific location. This may cause more profound complications such as personality changes, but electrode misplacement is relatively easy to identify using CT scan. Also, complications of surgery may occur, such as bleeding within the brain. After surgery, swelling of the brain tissue, mild disorientation, and sleepiness are normal. After 2–4 weeks, a follow-up visit is used to remove sutures, turn on the neurostimulator, and program it.[citation needed]
Because the brain can shift slightly during surgery, the electrodes can become displaced or dislodged from the specific location. This may cause more profound complications such as personality changes, but electrode misplacement is relatively easy to identify using CT scan. Also, complications of surgery may occur, such as bleeding within the brain. After surgery, swelling of the brain tissue, mild disorientation, and sleepiness are normal. After 2–4 weeks, a follow-up visit is used to remove sutures, turn on the neurostimulator, and program it.
因为在手术过程中大脑可能会轻微移动,电极可能会从特定位置移位或移位。这可能会导致更深刻的并发症,如个性(personality )的改变,但电极错位使用CT扫描(CT scan)相对容易识别。此外,手术并发症也可能发生,如脑出血。手术后,脑组织肿胀、轻度定向障碍和嗜睡均属正常。2-4周后,进行随访,拆除缝合线,打开神经刺激器,并对其进行编程。
Impaired swimming skills surfaced as an unexpected risk of the procedure; several Parkinson's disease patients lost their ability to swim after receiving deep brain stimulation.[24][25]
Impaired swimming skills surfaced as an unexpected risk of the procedure; several Parkinson's disease patients lost their ability to swim after receiving deep brain stimulation.
游泳技能受损被认为是该手术的一个意外风险;几名帕金森氏症患者在接受脑深部刺激后失去了游泳能力[24][25]。
Mechanisms
The exact mechanism of action of DBS is not known.[26] A variety of hypotheses try to explain the mechanisms of DBS:[27][28]
The exact mechanism of action of DBS is not known. A variety of hypotheses try to explain the mechanisms of DBS:
DBS 的确切作用机制尚不清楚[26] 。各种各样的假说试图解释 DBS 的机制:[27][28]
- Depolarization blockade: Electrical currents block the neuronal output at or near the electrode site.
- Synaptic inhibition: This causes an indirect regulation of the neuronal output by activating axon terminals with synaptic connections to neurons near the stimulating electrode.
- Desynchronization of abnormal oscillatory activity of neurons
- Antidromic activation either activating/blockading distant neurons or blockading slow axons[3]
- Depolarization blockade: Electrical currents block the neuronal output at or near the electrode site.
- Synaptic inhibition: This causes an indirect regulation of the neuronal output by activating axon terminals with synaptic connections to neurons near the stimulating electrode.
- Desynchronization of abnormal oscillatory activity of neurons
- Antidromic activation either activating/blockading distant neurons or blockading slow axons
- 去极化阻滞:电流阻断神经元在电极处或电极附近的输出。
- 突触抑制:通过激活与刺激电极附近的神经元突触连接的轴突末梢,引起神经元输出的间接调节。
- 神经元异常振荡活动的去同步。
- 反向激活激活/阻滞远端神经元或阻滞慢轴突[3]。
DBS represents an advance on previous treatments which involved pallidotomy (i.e., surgical ablation of the globus pallidus) or thalamotomy (i.e., surgical ablation of the thalamus).[29] Instead, a thin lead with multiple electrodes is implanted in the globus pallidus, nucleus ventralis intermedius thalami, or subthalamic nucleus, and electric pulses are used therapeutically. The lead from the implant is extended to the neurostimulator under the skin in the chest area.[citation needed]
DBS represents an advance on previous treatments which involved pallidotomy (i.e., surgical ablation of the globus pallidus) or thalamotomy (i.e., surgical ablation of the thalamus). Instead, a thin lead with multiple electrodes is implanted in the globus pallidus, nucleus ventralis intermedius thalami, or subthalamic nucleus, and electric pulses are used therapeutically. The lead from the implant is extended to the neurostimulator under the skin in the chest area.
DBS是对以往苍白球切开术( pallidotomy)(即,苍白球外科消融)或丘脑切开术(thalamotomy)(即,丘脑外科消融)治疗的一种进步[29] 。取而代之的是,将一个带有多个电极的细导线植入苍白球、腹外侧核(nucleus ventralis intermedius thalami)或丘脑下核( subthalamic nucleus),电脉冲用于治疗。植入物的导线延伸到胸部皮肤下的神经刺激器(neurostimulator)。
Its direct effect on the physiology of brain cells and neurotransmitters is currently debated, but by sending high-frequency electrical impulses into specific areas of the brain, it can mitigate symptoms[30] and directly diminish the side effects induced by PD medications,[31]allowing a decrease in medications, or making a medication regimen more tolerable.[citation needed]
Its direct effect on the physiology of brain cells and neurotransmitters is currently debated, but by sending high-frequency electrical impulses into specific areas of the brain, it can mitigate symptoms and directly diminish the side effects induced by PD medications, allowing a decrease in medications, or making a medication regimen more tolerable.
它对脑细胞和神经递质(neurotransmitters)的直接影响目前还在争论中,但通过向大脑的特定区域发送高频电脉冲,它可以s减轻症状[30] ,直接减少帕金森病药物引起的副作用[31],使药物减少,或使药物治疗方案更容易忍受[citation needed]。
Components and placement
The DBS system consists of three components: the implanted pulse generator (IPG), the lead, and an extension. The IPG is a battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain that interfere with neural activity at the target site. The lead is a coiled wire insulated in polyurethane with four platinum-iridium electrodes and is placed in one or two different nuclei of the brain. The lead is connected to the IPG by an extension, an insulated wire that runs below the skin, from the head, down the side of the neck, behind the ear, to the IPG, which is placed subcutaneously below the clavicle, or in some cases, the abdomen.[9] The IPG can be calibrated by a neurologist, nurse, or trained technician to optimize symptom suppression and control side effects.[32]
The DBS system consists of three components: the implanted pulse generator (IPG), the lead, and an extension. The IPG is a battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain that interfere with neural activity at the target site. The lead is a coiled wire insulated in polyurethane with four platinum-iridium electrodes and is placed in one or two different nuclei of the brain. The lead is connected to the IPG by an extension, an insulated wire that runs below the skin, from the head, down the side of the neck, behind the ear, to the IPG, which is placed subcutaneously below the clavicle, or in some cases, the abdomen.National Institute of Neurological Disorders and Stroke. Deep brain stimulation for Parkinson's disease information page Retrieved November 23, 2006. The IPG can be calibrated by a neurologist, nurse, or trained technician to optimize symptom suppression and control side effects.
DBS系统由三部分组成:植入脉冲发生器(IPG)、引线和扩展部分。IPG是一种由电池(battery)供电的神经刺激器,包裹在钛( titanium)外壳中,它向大脑发送电脉冲,干扰目标部位的神经活动(neural activity)。铅是用聚氨酯(polyurethane)绝缘的线圈,有四个铂铱(platinum-iridium)电极,被放置在大脑的一个或两个不同的核中。引线通过一根延伸线与IPG连接,这是一根绝缘电线,在皮肤下面,从头部、颈部侧面、耳朵后面,到IPG, IPG位于锁骨( clavicle)下皮下,在某些情况下,是腹部(abdomen)[9] 。IPG可以由神经科医生(neurologist)、护士( nurse)或训练有素的技术人员(technician)校准,以优化症状抑制和控制副作用[32]。
DBS leads are placed in the brain according to the type of symptoms to be addressed. For non-Parkinsonian essential tremor, the lead is placed in either the ventrointermediate nucleus of the thalamus or the zona incerta;[33] for dystonia and symptoms associated with PD (rigidity, bradykinesia/akinesia, and tremor), the lead may be placed in either the globus pallidus internus or the subthalamic nucleus; for OCD and depression to the nucleus accumbens; for incessant pain to the posterior thalamic region or periaqueductal gray; and for epilepsy treatment to the anterior thalamic nucleus.[34]
DBS leads are placed in the brain according to the type of symptoms to be addressed. For non-Parkinsonian essential tremor, the lead is placed in either the ventrointermediate nucleus of the thalamus or the zona incerta; for dystonia and symptoms associated with PD (rigidity, bradykinesia/akinesia, and tremor), the lead may be placed in either the globus pallidus internus or the subthalamic nucleus; for OCD and depression to the nucleus accumbens; for incessant pain to the posterior thalamic region or periaqueductal gray; and for epilepsy treatment to the anterior thalamic nucleus.Deep brain stimulation. Surgery Encyclopedia. Retrieved January 25, 2007.
根据需要治疗的症状类型,将DBS导联植入大脑。对于非帕金森特发性震颤,导线放置在丘脑(thalamus)腹中间核或内嵌带(zona incerta)[33]; 对于肌张力障碍和与PD相关的症状(强直(rigidity)、运动迟缓/运动不全( bradykinesia/akinesia)和震颤(tremor)),导线可置于苍白球内( globus pallidus internus)或丘脑下核(subthalamic nucleus);对强迫症和抑郁症的作用是伏隔核(nucleus accumbens);持续疼痛至丘脑后区或导水管周围灰质区( periaqueductal gray);以及丘脑前核( anterior thalamic nucleus)的癫痫治疗[34]。
All three components are surgically implanted inside the body. Lead implantation may take place under local anesthesia or under general anesthesia ("asleep DBS") such as for dystonia. A hole about 14 mm in diameter is drilled in the skull and the probe electrode is inserted stereotactically, using either frame-based or frameless stereotaxis.[35] During the awake procedure with local anesthesia, feedback from the person is used to determine the optimal placement of the permanent electrode. During the asleep procedure, intraoperative MRI guidance is used for direct visualization of brain tissue and device.[36] The installation of the IPG and extension leads occurs under general anesthesia.[37] The right side of the brain is stimulated to address symptoms on the left side of the body and vice versa.[citation needed]
All three components are surgically implanted inside the body. Lead implantation may take place under local anesthesia or under general anesthesia ("asleep DBS") such as for dystonia. A hole about 14 mm in diameter is drilled in the skull and the probe electrode is inserted stereotactically, using either frame-based or frameless stereotaxis. During the awake procedure with local anesthesia, feedback from the person is used to determine the optimal placement of the permanent electrode. During the asleep procedure, intraoperative MRI guidance is used for direct visualization of brain tissue and device. The installation of the IPG and extension leads occurs under general anesthesia.Deep Brain Stimulation, Department of Neurological Surgery, University of Pittsburgh. Retrieved May 13, 2008. The right side of the brain is stimulated to address symptoms on the left side of the body and vice versa.
这三种成分都要通过手术植入体内。铅植入可在局部麻醉或全身麻醉下进行(“睡眠DBS”),如肌张力障碍。在颅骨上钻一个直径约14毫米的孔,使用基于框架或无框架的立体定向(stereotactically)方式将探针电极立体定向插入[35]。在局部麻醉的清醒过程中,来自人的反馈被用来确定永久电极的最佳放置位置。在睡眠过程中,利用术中MRI引导对脑组织和设备进行直接可视化[36] 。IPG和延伸导线的安装是在全身麻醉下进行的[37]。刺激右脑来解决身体左侧的症状,反之亦然[citation needed]。
Research
Chronic pain
Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some people, but results vary. One study[38] of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.[39] DBS has also been applied for phantom limb pain.[40]
Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some people, but results vary. One study of 17 people with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life. DBS has also been applied for phantom limb pain.
刺激导水管周围灰质( periaqueductal gray)和脑室周围灰质( periventricular gray )来治疗痛觉性疼痛(nociceptive pain),刺激内囊( internal capsule)、腹侧后外侧核( ventral posterolateral nucleus)和腹侧后内侧核(ventral posteromedial nucleus)来治疗神经性疼痛(neuropathic pain),对一些人产生了令人印象深刻的结果,但结果各不相同。一项[38] 针对17名癌症顽固性疼痛患者的研究发现,其中13人几乎没有疼痛,只有4人在干预后出院时需要服用阿片类镇痛药。大多数人最终诉诸于阿片类药物,通常是在生命的最后几周[39] 。DBS也被用于治疗幻肢疼痛(phantom limb pain)[40]。
Major depression and obsessive-compulsive disorder

DBS has been used in a small number of clinical trials to treat people with severe treatment-resistant depression (TRD).[41] A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus,[42] nucleus accumbens,[43] ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula.[41] A recently proposed target of DBS intervention in depression is the superolateral branch of the medial forebrain bundle; its stimulation lead to surprisingly rapid antidepressant effects.[44]
DBS has been used in a small number of clinical trials to treat people with severe treatment-resistant depression (TRD). A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus, nucleus accumbens, ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula. A recently proposed target of DBS intervention in depression is the superolateral branch of the medial forebrain bundle; its stimulation lead to surprisingly rapid antidepressant effects.
DBS已在少量临床试验中用于治疗严重难治性抑郁症(treatment-resistant depression)(TRD)患者[41] 。DBS治疗TRD的神经解剖学靶点包括膝下扣带回、后直回[42]、伏隔核[43] 、腹侧囊/腹侧纹状体、丘脑下蒂和外侧缰状核[41] 。最近提出的DBS干预抑郁症的靶点是内侧前脑束(medial forebrain bundle)的上外侧支;它的刺激导致惊人的快速抗抑郁作用[44]。
The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target.[41] Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective treatment modality in the future.[45] In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment.[46][47][48]
The small numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target. Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective treatment modality in the future. In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which people who were deeply depressed were provided with portable stimulators for self treatment.
DBS治疗TRD的早期试验数量较少,目前限制了最佳神经解剖学靶点的选择[41] 。证据不足以支持DBS作为抑郁症的治疗方式;然而,该手术可能是未来一种有效的治疗方式(treatment modality)[45]。事实上,神经外科文献中已经记录了有益的结果,包括一些为重度抑郁的人提供便携式刺激器进行自我治疗的例子[46][47][48]。
A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders.[49] The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study.[50] However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders).[51] Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients.[52] Based on these results the Food and Drug Administration (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so.
A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger age of the psychiatric population relative to the age of people with movement disorders. The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study. However, a second randomized controlled study of ventral capsule DBS for TRD did demonstrate a significant difference in response rates between active DBS (44% responders) and sham DBS (0% responders). Efficacy of DBS is established for OCD, with on average 60% responders in severely ill and treatment-resistant patients. Based on these results the Food and Drug Administration (FDA) has approved DBS for treatment-resistant OCD under a Humanitarian Device Exemption (HDE), requiring that the procedure be performed only in a hospital with specialist qualifications to do so.
一项针对TRD和OCD的系统回顾发现了23例DBS, 9例为OCD, 7例为TRD, 1例为两者。“大约一半的患者确实表现出了显著的改善”,而且考虑到精神病患者的年龄相对于运动障碍患者的年龄,不良事件“通常微不足道”[49] 。在第一个随机对照研究中,DBS用于治疗以腹侧囊/腹侧纹状体区域为靶点的TRD,在16周的研究结束时,active组和sham组之间的缓解率没有显著差异[50]。然而,另一项腹侧胶囊DBS治疗TRD的随机对照研究确实表明,有效DBS(有效率为44%)和假DBS(有效率为0%)的缓解率存在显著差异)[51] 。DBS治疗强迫症疗效显著,重症和难治性患者平均有效率为60%[52]。根据这些结果,美国食品和药物管理局(Food and Drug Administration )(FDA)根据人道主义器械豁免(HDE)批准了DBS治疗顽症,要求只有在有专业资格的医院才能实施该手术。
DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality".[53]
DBS for TRD can be as effective as antidepressants and can have good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality".
DBS治疗TRD与抗抑郁药一样有效,有良好的反应率和缓解率,但不良反应和安全性必须得到更全面的评估。常见的副作用包括“伤口感染、围手术期头痛、情绪恶化/烦躁以及自杀倾向增加”[53]。
Other clinical applications
Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases.[54] The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication.[55] DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.[citation needed]
Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases. The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication. DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.
DBS对肌张力障碍患者的治疗结果显示,积极效果往往在数周至数月的时间内逐渐显现,至少在某些情况下显示出功能重组的作用[54] 。该方法已经在对药物有抗药性的癫痫(epilepsy)患者身上进行了有效性测试[55] 。DBS可通过程序性或反应性刺激减少或消除癫痫发作.[citation needed]。
DBS of the septal areas of persons with schizophrenia have resulted in enhanced alertness, cooperation, and euphoria.[56] Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.[47]
DBS of the septal areas of persons with schizophrenia have resulted in enhanced alertness, cooperation, and euphoria. Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.
对精神分裂症患者(schizophrenia)的鼻中隔区域(septal areas)进行DBS可增强警惕性、合作性和欣快感[54] 。有嗜睡症(narcolepsy )和复杂部分性癫痫(complex-partial seizures)的患者也报告说,自我诱发的间隔核深部脑刺激能产生欣快感和性想法[47]。
Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA.[57]
Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA.
据报道,通过深度电极对大脑进行电刺激,左侧海马体( hippocampus )为3毫安,右侧海马体(hippocampus)为1毫安[57]。
In 2015, a group of Brazilian researchers led by neurosurgeon 模板:Ill described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.[58]
In 2015, a group of Brazilian researchers led by neurosurgeon described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.
2015年,由神经外科医生领导的一组巴西研究人员描述了一种新技术,该技术允许同时植入电极,称为双侧立体定向术。主要的好处是花在手术上的时间更少,准确性更高[58]。
In 2016, DBS was found to improve learning and memory in a mouse model of Rett syndrome.[59] More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis,[60] making some first steps at explaining the restoration of hippocampal circuit function.
In 2016, DBS was found to improve learning and memory in a mouse model of Rett syndrome. More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis, making some first steps at explaining the restoration of hippocampal circuit function.
2016年,DBS被发现可以改善Rett综合征(Rett syndrome)小鼠模型的学习和记忆[59] 。最近2018年的研究表明,穹穴DBS上调了涉及突触功能、细胞存活和神经发生的基因[60] ,在解释海马回路功能的恢复方面迈出了一些第一步。
See also
- Brain implant
- Electroconvulsive therapy
- Electroencephalography
- Neuromodulation (medicine)
- Neuroprosthetics
- Organization for Human Brain Mapping
- Responsive neurostimulation device
- Robert G. Heath
- 模板:Interlanguage link multi
- Brain implant
- Electroconvulsive therapy
- Electroencephalography
- Neuromodulation (medicine)
- Neuroprosthetics
- Organization for Human Brain Mapping
- Responsive neurostimulation device
- Robert G. Heath
- 植入大脑
- 电痉挛疗法
- 脑电图
- 神经调节(医学)
- 神经修复
- 人脑映射组织
- 响应性神经刺激疗法设备
- Robert g. Heath
References
- ↑ 1.0 1.1 1.2 1.3 Kringelbach ML, Jenkinson N, Owen SL, Aziz TZ (August 2007). "Translational principles of deep brain stimulation". Nature Reviews. Neuroscience. 8 (8): 623–35. doi:10.1038/nrn2196. PMID 17637800. S2CID 147427108.
- ↑ 2.0 2.1 Hammond C, Ammari R, Bioulac B, Garcia L (November 2008). "Latest view on the mechanism of action of deep brain stimulation" (PDF). Movement Disorders. 23 (15): 2111–21. doi:10.1002/mds.22120. PMID 18785230. S2CID 14905206.
- ↑ 3.0 3.1 3.2 3.3 García MR, Pearlmutter BA, Wellstead PE, Middleton RH (2013). "A slow axon antidromic blockade hypothesis for tremor reduction via deep brain stimulation". PLOS ONE. 8 (9): e73456. Bibcode:2013PLoSO...873456G. doi:10.1371/journal.pone.0073456. PMC 3774723. PMID 24066049.
- ↑ 4.0 4.1 "FDA approves brain implant to help reduce Parkinson's disease and essential tremor symptoms". FDA. Retrieved May 23, 2016.
The first device, Medtronic’s Activa Deep Brain Stimulation Therapy System, was approved in 1997 for tremor associated with essential tremor and Parkinson’s disease.
- ↑ 5.0 5.1 'Brain pacemaker' treats dystonia. KNBC TV, April 22, 2003. Retrieved October 18, 2006.
- ↑ 6.0 6.1 "Medtronic Receives FDA Approval for Deep Brain Stimulation Therapy for Medically Refractory Epilepsy". newsroom.medtronic.com. Retrieved 2018-12-18.
- ↑ 7.0 7.1 "FDA Approves Humanitarian Device Exemption for Deep Brain Stimulator for Severe Obsessive-Compulsive Disorder". FDA.
- ↑ 8.0 8.1 Gildenberg PL (2005). "Evolution of neuromodulation". Stereotactic and Functional Neurosurgery. 83 (2–3): 71–79. doi:10.1159/000086865. PMID 16006778. S2CID 20234898.
- ↑ 9.0 9.1 9.2 9.3 National Institute of Neurological Disorders and Stroke. Deep brain stimulation for Parkinson's disease information page -{zh-cn:互联网档案馆; zh-tw:網際網路檔案館; zh-hk:互聯網檔案館;}-的存檔,存档日期2016-11-20. Retrieved November 23, 2006.
- ↑ 10.0 10.1 U.S. Department of Health and Human Services. FDA approves implanted brain stimulator to control tremors. Retrieved February 10, 2015.
- ↑ 11.0 11.1 Koller, W. and Melamed, E., 2007. Parkinson's disease and related disorders. 1st ed. Edinburgh: Elsevier.
- ↑ 12.0 12.1 Bronstein JM, et al. (February 2011). "Deep brain stimulation for Parkinson disease: an expert consensus and review of key issues". Archives of Neurology. 68 (2): 165. doi:10.1001/archneurol.2010.260. PMC 4523130. PMID 20937936.
- ↑ 13.0 13.1 Dallapiazza, R. F.; Vloo, P. D.; Fomenko, A.; Lee, D. J.; Hamani, C.; Munhoz, R. P.; Hodaie, M.; Lozano, A. M. et al. (2018). "Considerations for Patient and Target Selection in Deep Brain Stimulation surgery for Parkinson’s disease". In Stoker, T. B.; Greenland, J. C.. Parkinson's disease: Pathogenesis and clinical aspects. Brisbane: Codon Publications. doi:10.15586/codonpublications.parkinsonsdisease.2018.ch8. ISBN 978-0-9944381-6-4. PMID 30702838.
- ↑ 14.0 14.1 14.2 14.3 "Tourette syndrome and other tic disorders". Hyperkinetic Movement Disorders. 100. March 2005. pp. 641–57. doi:10.1016/B978-0-444-52014-2.00046-X. ISBN 9780444520142. PMID 21496613. Also see Singer HS (March 2005). "Tourette's syndrome: from behaviour to biology". The Lancet. Neurology. 4 (3): 149–59. doi:10.1016/S1474-4422(05)01012-4. PMID 15721825. S2CID 20181150.
- ↑ 15.0 15.1 15.2 15.3 Robertson MM (February 2011). "Gilles de la Tourette syndrome: the complexities of phenotype and treatment". British Journal of Hospital Medicine. 72 (2): 100–07. doi:10.12968/hmed.2011.72.2.100. PMID 21378617.
- ↑ 16.0 16.1 16.2 16.3 Du JC, Chiu TF, Lee KM, Wu HL, Yang YC, Hsu SY, Sun CS, Hwang B, Leckman JF (October 2010). "Tourette syndrome in children: an updated review". Pediatrics and Neonatology. 51 (5): 255–64. doi:10.1016/S1875-9572(10)60050-2. PMID 20951354.
- ↑ 17.0 17.1 Tourette Syndrome Association. Statement: Deep Brain Stimulation and Tourette Syndrome. Retrieved November 22, 2005.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 Malone DA, Pandya MM (2006). "Behavioral neurosurgery". Advances in Neurology. 99: 241–47. PMID 16536372.
- ↑ 19.0 19.1 Mink JW, Walkup J, Frey KA, Como P, Cath D, Delong MR, Erenberg G, Jankovic J, Juncos J, Leckman JF, Swerdlow N, Visser-Vandewalle V, Vitek JL (November 2006). "Patient selection and assessment recommendations for deep brain stimulation in Tourette syndrome" (PDF). Movement Disorders. 21 (11): 1831–38. doi:10.1002/mds.21039. hdl:2027.42/55891. PMID 16991144. S2CID 16353255.
- ↑ Viswanathan A, Jimenez-Shahed J, Baizabal Carvallo JF, Jankovic J (2012). "Deep brain stimulation for Tourette syndrome: target selection". Stereotactic and Functional Neurosurgery. 90 (4): 213–24. doi:10.1159/000337776. PMID 22699684.
- ↑ 21.0 21.1 Doshi PK (April 2011). "Long-term surgical and hardware-related complications of deep brain stimulation". Stereotactic and Functional Neurosurgery. 89 (2): 89–95. doi:10.1159/000323372. PMID 21293168. S2CID 10553177.
- ↑ 22.0 22.1 Scangos, K.W., Makhoul, G.S., Sugrue, L.P. (2021). "State-dependent responses to intracranial brain stimulation in a patient with depression". Nat Med. 27 (2): 229–231. doi:10.1038/s41591-020-01175-8. ISSN 1078-8956. PMC 8284979. PMID 33462446.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ 23.0 23.1 Burn DJ, Tröster AI (September 2004). "Neuropsychiatric complications of medical and surgical therapies for Parkinson's disease". Journal of Geriatric Psychiatry and Neurology. 17 (3): 172–80. doi:10.1177/0891988704267466. PMID 15312281.
- ↑ 24.0 24.1 "Deep Brain Stimulation May Put Parkinson's Patients at Risk for Drowning". www.medpagetoday.com (in English). 2019-11-27. Retrieved 2019-12-09.
- ↑ 25.0 25.1 Bangash, Omar K.; Thorburn, Megan; Garcia-Vega, Jimena; Walters, Susan; Stell, Rick; Starkstein, Sergio E.; Lind, Christopher R. P. (May 2016). "Drowning hazard with deep brain stimulation: case report". Journal of Neurosurgery. 124 (5): 1513–16. doi:10.3171/2015.5.JNS15589. ISSN 1933-0693. PMID 26566200.
- ↑ 26.0 26.1 Mogilner A.Y.; Benabid A.L.; Rezai A.R. (2004). "Chronic Therapeutic Brain Stimulation: History, Current Clinical Indications, and Future Prospects". Bioelectromagnetic medicine. New York: Marcel Dekker. pp. 133–51. ISBN 978-0-8247-4700-8.
- ↑ 27.0 27.1 McIntyre CC, Thakor NV (2002). "Uncovering the mechanisms of deep brain stimulation for Parkinson's disease through functional imaging, neural recording, and neural modeling". Critical Reviews in Biomedical Engineering. 30 (4–6): 249–81. doi:10.1615/critrevbiomedeng.v30.i456.20. PMID 12739751.
- ↑ 28.0 28.1 Herrington TM, Cheng JJ, Eskandar EN (January 2016). "Mechanisms of deep brain stimulation". Journal of Neurophysiology. 115 (1): 19–38. doi:10.1152/jn.00281.2015. PMC 4760496. PMID 26510756.
- ↑ 29.0 29.1 Machado A, Rezai AR, Kopell BH, Gross RE, Sharan AD, Benabid AL (June 2006). "Deep brain stimulation for Parkinson's disease: surgical technique and perioperative management". Movement Disorders. 21 Suppl 14 (Suppl 14): S247–58. doi:10.1002/mds.20959. PMID 16810722. S2CID 18194178.
- ↑ 30.0 30.1 Moro E, Lang AE (November 2006). "Criteria for deep-brain stimulation in Parkinson's disease: review and analysis". Expert Review of Neurotherapeutics. 6 (11): 1695–705. doi:10.1586/14737175.6.11.1695. PMID 17144783. S2CID 20857769.
- ↑ 31.0 31.1 Apetauerova D, Ryan RK, Ro SI, Arle J, Shils J, Papavassiliou E, Tarsy D (August 2006). "End of day dyskinesia in advanced Parkinson's disease can be eliminated by bilateral subthalamic nucleus or globus pallidus deep brain stimulation". Movement Disorders. 21 (8): 1277–79. doi:10.1002/mds.20896. PMID 16637040. S2CID 42122286.
- ↑ 32.0 32.1 Volkmann J, Herzog J, Kopper F, Deuschl G (2002). "Introduction to the programming of deep brain stimulators". Movement Disorders. 17 Suppl 3: S181–87. doi:10.1002/mds.10162. PMID 11948775. S2CID 21988668.
- ↑ 33.0 33.1 Lee JY, Deogaonkar M, Rezai A (July 2007). "Deep brain stimulation of globus pallidus internus for dystonia". Parkinsonism & Related Disorders. 13 (5): 261–65. doi:10.1016/j.parkreldis.2006.07.020. PMID 17081796.
- ↑ 34.0 34.1 Deep brain stimulation. Surgery Encyclopedia. Retrieved January 25, 2007.
- ↑ 35.0 35.1 Owen CM, Lindsey ME (May 2009). "Frame-based stereotaxy in a frameless era: current capabilities, relative role, and the positive- and negative predictive values of blood through the needle". Journal of Neuro-Oncology. 93 (1): 139–49. doi:10.1007/s11060-009-9871-y. PMID 19430891.
- ↑ 36.0 36.1 Starr PA, Martin AJ, Ostrem JL, Talke P, Levesque N, Larson PS (March 2010). "Subthalamic nucleus deep brain stimulator placement using high-field interventional magnetic resonance imaging and a skull-mounted aiming device: technique and application accuracy". Journal of Neurosurgery. 112 (3): 479–90. doi:10.3171/2009.6.JNS081161. PMC 2866526. PMID 19681683.
- ↑ 37.0 37.1 Deep Brain Stimulation, Department of Neurological Surgery, University of Pittsburgh. Retrieved May 13, 2008.
- ↑ 38.0 38.1 Young RF & Brechner T (1986). "Electrical stimulation of the brain for relief of intractable pain due to cancer". Cancer. 57 (6): 1266–72. doi:10.1002/1097-0142(19860315)57:6<1266::aid-cncr2820570634>3.0.co;2-q. PMID 3484665.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ 39.0 39.1 Johnson MI, Oxberry SG & Robb K (2008). "Stimulation-induced analgesia". In Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain (2nd ed.). London: Hodder Arnold. pp. 235–50. ISBN 978-0-340-94007-5.
- ↑ 40.0 40.1 Kringelbach ML, Jenkinson N, Green AL, Owen SL, Hansen PC, Cornelissen PL, Holliday IE, Stein J, Aziz TZ (February 2007). "Deep brain stimulation for chronic pain investigated with magnetoencephalography". NeuroReport. 18 (3): 223–28. CiteSeerX 10.1.1.511.2667. doi:10.1097/wnr.0b013e328010dc3d. PMID 17314661. S2CID 7091307.
- ↑ 41.0 41.1 41.2 41.3 41.4 41.5 Anderson RJ, Frye MA, Abulseoud OA, Lee KH, McGillivray JA, Berk M, Tye SJ (September 2012). "Deep brain stimulation for treatment-resistant depression: efficacy, safety and mechanisms of action". Neuroscience and Biobehavioral Reviews. 36 (8): 1920–33. doi:10.1016/j.neubiorev.2012.06.001. PMID 22721950. S2CID 207089716.
- ↑ 42.0 42.1 Accolla EA, Aust S, Merkl A, Schneider GH, Kühn AA, Bajbouj M, Draganski B (April 2016). "Deep brain stimulation of the posterior gyrus rectus region for treatment resistant depression". Journal of Affective Disorders. 194: 33–37. doi:10.1016/j.jad.2016.01.022. PMID 26802505.
- ↑ 43.0 43.1 Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, Joe AY, Kreft M, Lenartz D, Sturm V (January 2008). "Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression". Neuropsychopharmacology. 33 (2): 368–77. doi:10.1038/sj.npp.1301408. PMID 17429407.
- ↑ 44.0 44.1 Schlaepfer TE, Bewernick BH, Kayser S, Mädler B, Coenen VA (June 2013). "Rapid effects of deep brain stimulation for treatment-resistant major depression". Biological Psychiatry. 73 (12): 1204–12. doi:10.1016/j.biopsych.2013.01.034. PMID 23562618. S2CID 6374368.
- ↑ 45.0 45.1 Murphy, Destiny N.; Boggio, Paulo; Fregni, Felipe (2009). "Transcranial direct current stimulation as a therapeutic tool for the treatment of major depression: insights from past and recent clinical studies". Curr Opin Psychiatry. 22 (3): 306–11. doi:10.1097/YCO.0b013e32832a133f. PMID 19339889. S2CID 11392351.
- ↑ 46.0 46.1 Delgado, Jose (1986). Physical Control of the Mind: Toward a Psychocivilized Society. New York: Harper and Row. ISBN 0-06-131914-7.
- ↑ 47.0 47.1 47.2 47.3 Faria MA (2013). "Violence, mental illness, and the brain – A brief history of psychosurgery: Part 3 – From deep brain stimulation to amygdalotomy for violent behavior, seizures, and pathological aggression in humans". Surgical Neurology International. 4 (1): 91. doi:10.4103/2152-7806.115162. PMC 3740620. PMID 23956934.
- ↑ 48.0 48.1 Robison RA, Taghva A, Liu CY, Apuzzo ML (2012). "Surgery of the mind, mood, and conscious state: an idea in evolution". World Neurosurgery. 77 (5–6): 662–86. doi:10.1016/j.wneu.2012.03.005. PMID 22446082.
- ↑ 49.0 49.1 Lakhan SE, Callaway E (March 2010). "Deep brain stimulation for obsessive-compulsive disorder and treatment-resistant depression: systematic review". BMC Research Notes. 3 (1): 60. doi:10.1186/1756-0500-3-60. PMC 2838907. PMID 20202203.
- ↑ 50.0 50.1 Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O'Reardon JP, Eskandar EN, Baltuch GH, Machado AD, Kondziolka D, Cusin C, Evans KC, Price LH, Jacobs K, Pandya M, Denko T, Tyrka AR, Brelje T, Deckersbach T, Kubu C, Malone DA (August 2015). "A Randomized Sham-Controlled Trial of Deep Brain Stimulation of the Ventral Capsule/Ventral Striatum for Chronic Treatment-Resistant Depression". Biological Psychiatry. 78 (4): 240–48. doi:10.1016/j.biopsych.2014.11.023. PMID 25726497. S2CID 22644265.
- ↑ 51.0 51.1 Bergfeld IO, Mantione M, Hoogendoorn ML, Ruhé HG, Notten P, van Laarhoven J, et al. (May 2016). "Deep Brain Stimulation of the Ventral Anterior Limb of the Internal Capsule for Treatment-Resistant Depression: A Randomized Clinical Trial". JAMA Psychiatry. 73 (5): 456–64. doi:10.1001/jamapsychiatry.2016.0152. PMID 27049915.
- ↑ 52.0 52.1 Alonso P, Cuadras D, Gabriëls L, Denys D, Goodman W, Greenberg BD, et al. (2015-07-24). "Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Meta-Analysis of Treatment Outcome and Predictors of Response". PLOS ONE. 10 (7): e0133591. Bibcode:2015PLoSO..1033591A. doi:10.1371/journal.pone.0133591. PMC 4514753. PMID 26208305.
- ↑ 53.0 53.1 Moreines JL, McClintock SM, Holtzheimer PE (January 2011). "Neuropsychologic effects of neuromodulation techniques for treatment-resistant depression: a review". Brain Stimulation. 4 (1): 17–27. doi:10.1016/j.brs.2010.01.005. PMC 3023999. PMID 21255751.
- ↑ 54.0 54.1 54.2 Krauss JK (2002). "Deep brain stimulation for dystonia in adults. Overview and developments". Stereotactic and Functional Neurosurgery. 78 (3–4): 168–82. doi:10.1159/000068963. PMID 12652041. S2CID 71888143.
- ↑ 55.0 55.1 Wu C, Sharan AD (Jan–Feb 2013). "Neurostimulation for the treatment of epilepsy: a review of current surgical interventions". Neuromodulation. 16 (1): 10–24, discussion 24. doi:10.1111/j.1525-1403.2012.00501.x. PMID 22947069. S2CID 1711587.
- ↑ Heath RG (January 1972). "Pleasure and brain activity in man. Deep and surface electroencephalograms during orgasm". The Journal of Nervous and Mental Disease. 154 (1): 3–18. doi:10.1097/00005053-197201000-00002. PMID 5007439. S2CID 136706.
- ↑ 57.0 57.1 Surbeck W, Bouthillier A, Nguyen DK (2013). "Bilateral cortical representation of orgasmic ecstasy localized by depth electrodes". Epilepsy & Behavior Case Reports. 1: 62–65. doi:10.1016/j.ebcr.2013.03.002. PMC 4150648. PMID 25667829.
- ↑ 58.0 58.1 Fonoff ET, Azevedo A, Angelos JS, Martinez RC, Navarro J, Reis PR, Sepulveda ME, Cury RG, Ghilardi MG, Teixeira MJ, Lopez WO (July 2016). "Simultaneous bilateral stereotactic procedure for deep brain stimulation implants: a significant step for reducing operation time". Journal of Neurosurgery. 125 (1): 85–89. doi:10.3171/2015.7.JNS151026. PMID 26684776.
- ↑ 59.0 59.1 Lu H, Ash RT, He L, Kee SE, Wang W, Yu D, Hao S, Meng X, Ure K, Ito-Ishida A, Tang B, Sun Y, Ji D, Tang J, Arenkiel BR, Smirnakis SM, Zoghbi HY (August 2016). "Loss and Gain of MeCP2 Cause Similar Hippocampal Circuit Dysfunction that Is Rescued by Deep Brain Stimulation in a Rett Syndrome Mouse Model". Neuron. 91 (4): 739–47. doi:10.1016/j.neuron.2016.07.018. PMC 5019177. PMID 27499081.
- ↑ 60.0 60.1 Pohodich AE, Yalamanchili H, Raman AT, Wan YW, Gundry M, Hao S, Jin H, Tang J, Liu Z, Zoghbi HY (March 2018). "Forniceal deep brain stimulation induces gene expression and splicing changes that promote neurogenesis and plasticity". eLife. 7. doi:10.7554/elife.34031. PMC 5906096. PMID 29570050.
Further reading
- Appleby BS, Duggan PS, Regenberg A, Rabins PV (September 2007). "Psychiatric and neuropsychiatric adverse events associated with deep brain stimulation: A meta-analysis of ten years' experience". Movement Disorders. 22 (12): 1722–8. doi:10.1002/mds.21551. PMID 17721929. S2CID 22925963.
- Schlaepfer TE, Bewernick BH, Kayser S, Hurlemann R, Coenen VA (May 2014). "Deep brain stimulation of the human reward system for major depression--rationale, outcomes and outlook". Neuropsychopharmacology. 39 (6): 1303–14. doi:10.1038/npp.2014.28. PMC 3988559. PMID 24513970.
- Diamond A, Shahed J, Azher S, Dat-Vuong K, Jankovic J (May 2006). "Globus pallidus deep brain stimulation in dystonia". Movement Disorders. 21 (5): 692–5. doi:10.1002/mds.20767. PMID 16342255. S2CID 29677149.
- "Deep Brain Stimulation for Parkinson's Disease in Movement Disorders". Bioelectromagnetic medicine. New York, N.Y: Marcel Dekker. 2004. pp. 265–76. ISBN 978-0-8247-4700-8.
External links
- Video: Deep brain stimulation to treat Parkinson's disease
- Video: Deep brain stimulation therapy for Parkinson's disease
- The Perils of Deep Brain Stimulation for Depression. Author Danielle Egan. September 24, 2015.
- Treatment center for Deep Brain Stimulation of movement disorders, OCD, Tourette or depression.
- Treatment center for Deep Brain Stimulation for OCD
- Video: Deep brain stimulation to treat Parkinson's disease
- Video: Deep brain stimulation therapy for Parkinson's disease
- The Perils of Deep Brain Stimulation for Depression. Author Danielle Egan. September 24, 2015.
- Treatment center for Deep Brain Stimulation of movement disorders, OCD, Tourette or depression.
- Treatment center for Deep Brain Stimulation for OCD
- 视频: 脑深部电刺激治疗帕金森氏症
- 视频: 脑深部电刺激治疗帕金森氏症
- 脑深部电刺激治疗抑郁症的风险。作者丹妮尔 · 伊根。2015年9月24日。
- 脑深部电刺激治疗运动障碍、强迫症、抽动秽语综合症或抑郁症中心。
- 脑深部电刺激治疗强迫症中心
Category:Electrotherapy Category:Medical devices Category:Neurology procedures Category:Neuroprosthetics Category:Neurosurgical procedures Category:Neurotechnology Category:Tourette syndrome Category:1987 introductions
类别: 电子疗法类别: 医疗设备类别: 神经内科手术类别: 神经修复类别: 神经外科手术类别: 神经技术类别: 神经图雷特氏综合症类别: 1987年引言
This page was moved from wikipedia:en:Deep brain stimulation. Its edit history can be viewed at 深部脑刺激/edithistory
- Webarchive模板wayback链接
- CS1 maint: uses authors parameter
- CS1 English-language sources (en)
- CS1: long volume value
- Articles with short description
- All articles with unsourced statements
- Articles with unsourced statements from November 2013
- Articles with invalid date parameter in template
- Articles with unsourced statements from January 2017
- Electrotherapy
- Medical devices
- Neurology procedures
- Neuroprosthetics
- Neurosurgical procedures
- Neurotechnology
- Tourette syndrome
- 1987 introductions
- 待整理页面